Total hip replacement
Before surgery :
- Hip osteoarthritis and necrosis are the two major causes of the painful degradation of the hip joint. In both cases, the rubbing cartilage surface between the thighbone and pelvis cavity has been eroded. This causes pain and/or impairing stiffness.
- There’s no effective means today to repair this cartilaginous rubbing surface.
- For the surgeon to opt for a total hip replacement two conditions are required: both rough pain and/or discomfort, enduring and resistant to medical treatment and an x-ray of the hip that will confirm the evolved erosion.
- A thorough pre-operative assessment will be mandatory including: consulting an anaesthesiologist and a cardiologist; a blood test, a specific x-ray that will allow to take the dimensions of the required prosthesis.
During surgery :
- The skin incision is made on the edge to access the hip joint.
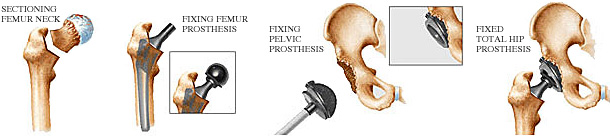
- The procedure mean duration is 1.30 hours : from the laying of operative fields to the exit of the operating theatre. The different operating times are charted in the 4 drawings below.
- A system of blood salvage system (cellsaver) makes it possible to re-inject to the patient the blood cells lost during the procedure.
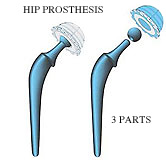
- A total hip artificial implant is made of 3 or 4 parts, some are fitted to the femoral and hip bone; others are assembled together. Metal, (various chrome- cobalt, titanium or oxinium alloys are available), ultra high density polyethylene and ceramics are the three most conventional materials used for a total hip implant. Besides, there are dozens of other types of artificial implants among which the surgeon takes his pick in accordance with every single case.
After surgery :
- Two days after surgery the patient is able to sit on a chair.
- Redon drains (small tubes inserted under the scar to let blood ooze and prevent clots) are removed on the third day.
- The patient can start walking with crutches as soon as possible in the days following the surgery to prevent phlebitis (blood clot inside a leg vein).
- On an average, the stay at the clinic lasts a week but tends to be shorter with the latest medical advances (cf. Next chapter).
- A rehabilitation programme becomes then necessary, it begins during the stay at the clinic and is carried on with a physiotherapist in a rehabilitation centre or at home for about 2 to 4 weeks.
- During the first months, a few domestic and positioning rules are to be respected to prevent the dislocation of the implant. This dislocation is much rarer when the whole tissues around the implant have healed, which can last 2 to 3 months. Driving is to be avoided during the first weeks after surgery for instance.
Latest breakthroughs :
- The latest materials developed are aimed at limiting the progressive erosion of the implant (Metasul® or Ceramics), and improving the fixation to the bone (Titane or Hydryoxiapatite) to prevent dislocation (double mobility cup).
- These innovative products allow to expect an implant life expectancy superior to the 15 years which are the usual duration expected today.
- These implants can be fixed today with or without cement; both options have got their benefits and disadvantages.
- New computer-assisted or non-assisted replacement techniques allow to place these modern implants by using a minimally invasive procedure i.e. by making a smaller incision, avoiding cutting muscles, limiting blood loss therefore logically leading to a faster recovery of the motion in your hip as well as walking. ( cf. Minimally invasive hip replacement ).
